Sex and Youths
If the care of transgender youths seems like a new issue, that’s because it is. And, if it feels as if it has also been a rapidly growing one, that’s because that is also true. In part because of this newness and rapid expansion, but also due to a lack of scientific rigor in the gender identity clinics caring for these children and adolescents, we have not established an adequate knowledge base of how best to care for these youths. Due to all these factors, newness, rapidity, and inadequate knowledge, pushback was inevitable, and long overdue.
I think the critiques of politicians and activists should be set aside, as they may have other motives for speaking out. But, there are three more credible sources of resistance: the scientific community, itself; concerned current and former transgender care providers; and those youths and adults who have regretted their prior decisions and realigned with their biologic gender, the desisters and detransitioners. I will present those counterpoints in my next post, but I first want to review a bit of history, as I think it is informative.

The modern era of the care of transgender youths began in the Netherlands in the 1980s and 1990s, and the “Dutch Protocol” was formally introduced in 2006. For children with gender dysphoria, counseling was performed, but it was not focused on the gender dysphoria, itself. Parents were encouraged to adopt an attitude of watchful waiting, as it was known that most gender dysphoric children would resolve their feelings of gender disparity by or during adolescence. Social transitioning was generally discouraged, because such decisions can lead to more social obstacles for the later adolescent to realign with his or her biological sex. This cautious approach to gender dysphoric children seems entirely appropriate to me.
For adolescents with persistent gender dysphoria, puberty blockers might be offered at the onset of physical changes associated with puberty, possibly followed by cross-sex hormones at around age 16. Gender reassignment surgeries were typically not offered until age 18. Unlike with the watchful waiting approach to gender dysphoric children, where there is scientific support, there isn’t good research to justify this care of gender dysphoric adolescents. As an aside, some of the early Dutch research was supported by the pharmaceutical manufacturer of the puberty blocker used in those studies; that isn’t necessarily wrong, but I still find it bothersome.
The first dedicated clinic for gender dysphoric American youths was established at Boston Children’s Hospital in 2007; today, we have more than 60 such clinics. While U.S. centers initially adopted the Dutch protocol, a “Gender Affirmative Model” was introduced in 2013. The authors didn’t lay out a specific guideline of care, but rather a philosophy of their approach to gender dysphoric and non-conforming youths, to “allow time and space for exploration and self-acceptance within an infinite variety of authentic gender selves”. This model takes the claims of even very young children at face value, and does not embrace the watchful waiting approach of the Dutch protocol. Near the end of the editorial, the authors ask multiple questions for which they agree we need answers, to include the consequences of receiving puberty blockers and cross-sex hormones; I found that paragraph refreshingly honest.
We didn’t have answers to those questions in 2013, and still do not. While there have been dozens of reports published in support of this protocol or that model, none have been scientifically rigorous, in the sense of proving or disproving a hypothesis, with adequate sample sizes, control groups, and treatment randomization. Instead, most are simply observational reports. These are perfectly acceptable, even necessary, but their primary purpose is to generate hypotheses that might later be verified or falsified. And, that has yet to be done.
Human Development, 2013: The Gender Affirmative Model: What We Know and What We Aim to Learn
American Psychological Association, 2018: Introduction to the Gender Affirmative Model

During this time, there was also a shift in how the medical community, and especially the psychiatric community, began to view gender issues. Transvestites became transexuals, and then transgender. Gender identity disorder, previously a mental health disorder, became gender dysphoria, now a personal identity rather than a psychiatric condition, and dysphoria, a feeling of discomfort with one’s own body, became less of a criteria for pursuing gender transitioning. A wonderful, almost metaphysical review of gender, sexuality, and psychiatry, is cited below, and well worth a read.
Cambridge University Press, 2020: Sex, Gender and Gender Identity: A Reevaluation of the Evidence
In addition to the unanswered questions of how best to care for gender dysphoric and non-conforming children and adolescents, we have seen a rapid increase in referrals to gender identity clinics around the world in the past decade. Although there have been many hypotheses advanced, to include the impact of mainstream media, the influence of online communities such as YouTube and Tumblr, and the possibility of social contagion within friend groups (especially biologic females), this phenomenon remains largely unexplained and concerning for many.
Reuters, 2022: A Gender Imbalance Emerges Among Trans Teens Seeking Treatment
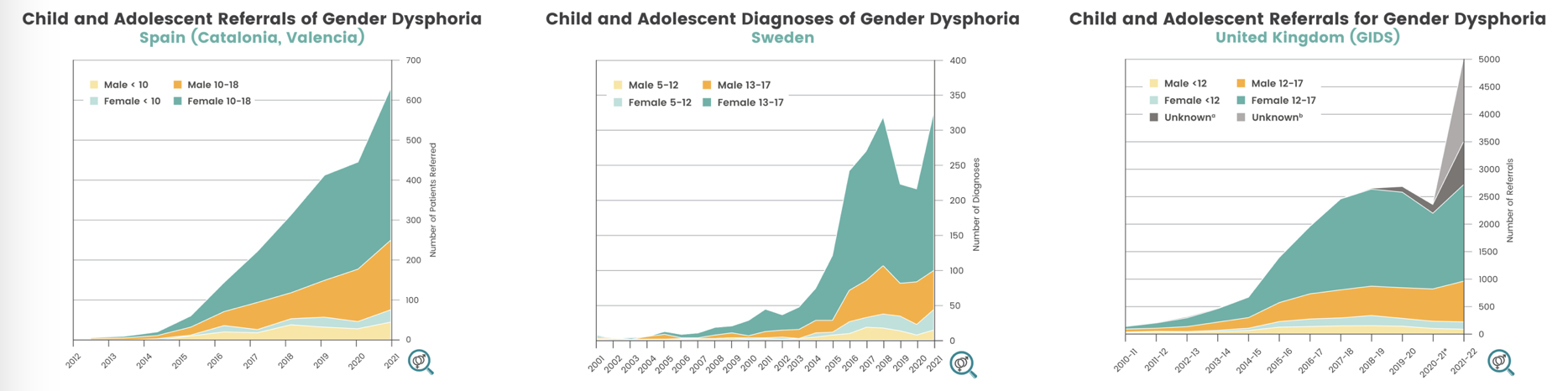
I could not find a comparable graph for referrals in the United States overall, but individual reports suggest a comparably rapid rise in the past decade has been experienced here, as well. The following citations give proof to this claim.
Reuters, 2022: Putting Numbers on the Rise in Children Seeking Gender Care
Williams Institute, 2022: How Many Adults and Youth Identify as Transgender in the United States?
The youth transgender movement is relatively new, it is growing rapidly, and we don’t have good data upon which to base care decisions. Still, from what we do know, I think we can make several safe assumptions to inform what our approach might be.
First, and perhaps most importantly, is how we should deal with gender dysphoric children. Here, I believe we should embrace the watchful waiting approach of the Dutch protocol, recognizing that the majority will desist by adolescence. We should not encourage social transitioning, as that can lead to more social obstacles should the child later realign with their natal sex. And while I think schools have a role to play in encouraging children to be more accepting and less inclined toward bullying generally, I don’t think they should be addressing issues of gender identity. This is especially true of primary school students, who are probably not capable of understanding these issues in a meaningful manner, anyway.
For children and adolescents alike, we should treat the whole of the person before us, not focus only on the gender dysphoria on non-conformity. Many of these youths have mental health problems, such as anxiety, depression, attention deficit disorders, autism spectrum disorders, and substance use disorders. They have a much higher incidence of suicidal ideation and self-inflicted injuries. Many have a history of sexual abuse or other adverse childhood experiences. From some reports, which we will get to in my next entry, it appears that these other issues, which may be the underlying reason for the purported gender dysphoria, are sometimes ignored, while the dysphoria is treated. Especially for female adolescents, counselors should consider the impact of social media, the possibility of social contagion within friend groups, and the understandable apprehension of becoming a woman in our overly sexualized culture.
We should avoid prescribing puberty blockers to prepubescent and adolescent youths. We don’t have clear data on the long term effects of preventing puberty to proceed naturally, and even studies of the purported benefits of puberty blockers to the mental health of gender dysphoric adolescents has been mixed. Apart from external bodily changes, brain maturation is an important part of puberty, and we don’t know how that is being affected. It is argued, but not proven, that puberty blockers are “totally reversible”, but this is almost certainly not the case. And, based upon observational reports, the majority of youths who receive puberty blockers will later proceed with cross-sex hormones, which have undeniably irreversible effects. Some youths treated with puberty blockers and cross-sex hormones will be made permanently infertile, and some may never experience an orgasm.
One downside of allowing puberty to proceed naturally is that transgender adults will have to deal with the persistence of secondary sexual characteristics of their biologic sex, such as facial hair or a deeper voice for transgender females. That’s not nothing, but still might be overall preferable to the challenges experienced by detransitioners, who have to deal with even greater changes, especially those who have undergone surgical transitioning. Furthermore, for those who remain comfortable with their decision to transition, the use of puberty blockers and cross-sex hormones in adolescence can make some surgical transitioning procedures more difficult later.
Surgical transitioning is something that I believe should only be performed on adults, and never on youths of any age. So called “top surgery”, mastectomy for natal females, and breast implants for natal males, are common. Removal of sexual organs, such as the uterus and ovaries for natal females and the testicles of natal males are also common. More advanced “bottom surgery”, creating a penis-like structure from the clitoris of natal females and a vagina-like structure from the penis and scrotum of natal males, is less common, due to the complexity of the procedures and associated complications.
It’s not at all clear to me how youths faced with such choices as puberty blockers, cross-sex hormones, or surgical transitioning can ever give truly informed consent. Many will have never experienced an orgasm or given much thought to being a parent or wanting to breastfeed one day. And, we know from other research that the human brain doesn’t fully mature until 23 to 25 years of age. These are hefty decisions we’re leaving to immature young people and to their concerned parents who want the best for their children, but may passively accept the advice of the clinician in the white coat.
Are we on the right path? Personally, I don’t think so, and I am certain that we don’t have good evidence to establish that we are. In my next installment, we’ll hear from the broader scientific community, current and former transgender care providers, and those who have regretted their decisions, the desisters and detransitioners.
Neuropsychiatric Disease and Treatment, 2013: Maturation of the Adolescent Brain
The Lancet, 2017: Puberty Suppression in Transgender Children and Adolescents
The New Atlantis, 2017: Growing Pains
Reuters, 2022: As More Transgender Children Seek Medical Care, Families Confront Many Unknowns
